Dr David Guex - Dr Jean-Yves Cochet
January 2016 - Magazine DT Study Club (vol 4 - N°1/2016)
May 2016 - Dental Tribune
Download the PDF
The age old problem of the ductal system disinfection is still on the table. The colonization of the root canal system is not without negligible effects, both in terms of its well-known induced diseases than immediate tissue destruction osseous and periodontal.
Various studies show the bacterial potential to survive in a disinfected, cleaned and filled in a tight manner. Figdor and al.[1] have shown that Enterococcus faecalis has the ability to survive in no nutrient environment and prosper when the source of nutritional element is restored. In an ex-vivo study, Sedgley and al.[2] have shown that enterococcus faecalis is able to recover from the state of prolonged famine (starvation) even sequestered in treated root canals, inoculated in the canals, in the absence of nutrient it still vital for 12 months and keeps its pathogenic potential.
Thus, the viable enterococcus faecalis at the time of the filling can provide in the long term a nest for a subsequent infection. In this context the variety of available files in the marketplace to activate the irrigation solutions shows that despite our best efforts we obviously do not have the desired results. Perhaps the word energy might be complementary called disinfection to become an indispensable synergy.
The heated hypochlorite is more efficient because the provided energy in the form of heat potentiates its effectiveness, just bringing energy to the irrigation solutions will allow:
- To vehicle them to the apex
- To diffuse them in the accessory canals.
- To make them more fluid
- To make them more active
As soon as a rotary file goes to the apex it creates 2 effects, a positive (beneficial) and the second a negative. The beneficial in fact is to a section of the contaminated dentin by bacteria via dentinal tubulars over several microns. The absence of that contaminated dentin will optimize the filling by a better adaptation. The negative effect is that any instrumental penetration causes a passage of air and a compression of this air in a closed system by the periodontal tissues if we have a vital tooth, or inflammatory, granulomatous even cystic if the tooth is necrotic. At this stage the air has fully penetrated into the canal and it will prevent the irrigants from diffusing to the apical area, the air cap is in place, it's the physical effect: ”Vapor Lock”.
The first records on the gas trapping effects or air in closed system were realized by Deutsch[3], from a theoretical point of view and Pesse and al.[4] from an experimental version. The irrigation solution delivered to the syringe without wedging the needle into the canal does not go further the tip of the needle, because of the presence of the air column[5] of which surprisingly, one rediscovers the importance today[6]. Since then many articles have described the effect of vapor lock in the canals and in one side closed tubes, by suggesting that due to the atmospheric pressure when an irritant is introduced inside the solution is prevented from reaching the end[7]. The physical parameters affecting the air trapped in the canal is the angle contact of the liquid and the walls angle of the canal[8]. For example a canal with wall angle having a closed angle does not allow the irrigation fluid to discharge the entrapped air. A possible way to get rid of the initial bubbles is the use of a permeability file, since the results of this study[9] showed that maintaining apical permeability in wide canals leads to significantly minimize the presence of gas bubbles in the middle thirds and cervical. But this study is about the wide canals, then what happens with the narrow ones?
By making test on transparent teeth according the Augusto Malentacca technique, the solutions diffuse very poorly towards the apex. As soon as we irrigate an instrumented canal, there is always an air bubble in the apical area. Thanks to the use of the permeability file between each manual or rotary file, we manage to move it, but it's impossible to get rid of it (eliminate it)[9bis].
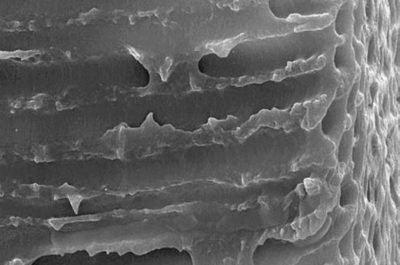
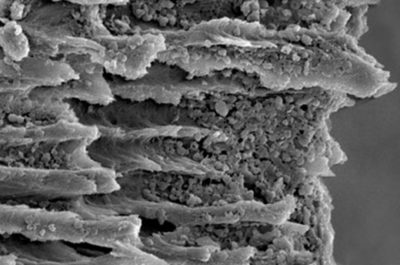
Unfortunately to the exclusion of a few monoradiculates teeth, we are dealing with a complex root cana system. This endodontic anatomy has been demonstrated in 1925 by the W. Hess boards made out of Chinese ink[10]. Peters[11] shows that " on the maxillary molar, whatever technique used more than 35% of the ductal surfaces remain not instrumented ".This physical and anatomical problem is complicated by the bacterial colonization of this labyrinthine canal system.
In the first stage the bacteria progress by divisions rather by displacement[12]. It means that in order to reach the apex, the number must increase. And what we find at the apex are the most pathogenic bacteria[13]. Thus, the conjunction between endodontic anatomy and the degree of bacterial contamination shows (reveals) that we will need an irrigation energy and for destructuring the bacterial biofilm and for diffusing our products into the dentinal tubules. And the more bacteria have been in place for a long time, the more resistant they are thanks to a protective system: the bacteria biofilm. Because obviously we'll give them time, bacteria will organize into a biofilm. A biofilm is constituted approximately by a volume of 15% bacteria and 85% Matrix[14]. The endodontic flora includes more than 500 species and this biofilm becomes 1000 to 2000 times more resistant to antiseptic solutions[15]. For example the necessary concentration of antibiotics to kill strain in a biofilm is 250 times more important than a planktonic growth bacterial strain[16]. The conclusion of this study shows that our major problem is the weak contact of irrigation solutions on the dentinal walls in the apical area, the all thing correlated to 2 major problems.
- The most pathogenic bacteria are located in the last apical millimeters[13bis].
- The bacteria are both located along the walls but also inside the dentinal tubules in-depths ranging from 300 to 1500 um[17].
When we talked about transmitted energy to irrigation solutions, we can think of the energy delivered by different systems, including lasers. There are several different lasers but actually a bundle of studies focuses on the use of the Erbium YAG laser. Indeed from Hirono Takeda showed that in endodontics the most efficient laser was the Erbium YAG laser for the removal of debris and smear layer[18]. How can we explain these results?
When we plunge the fiber contained in the pulp chamber and press the pedal of the machine, the chamber generates a series of excited photons at a precise wavelength 2940 nm. The molecules intrinsically have absorption curves and it shows that this 2940 nm wavelength is maximally absorbed (= absorption peak) by water and hydroxy apatite. When 2940 nm excited photons encounter a water molecule this water molecule will be sublimated. The Erbium YAG laser works by the implosion of the molecules of water, this sublimation of water is called plasma (Fig. 1).
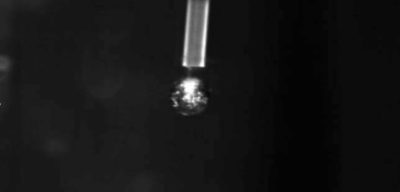
Water plasma corresponds to the fourth element constituting the universe, the three others being liquid, gaseous and solid elements. Our sun is a plasma. Actually plasma doesn't come out of the end of the tip, plasma is a transformation of matter by photonic energy. There are different plasmas: water plasma, dentin plasma and blood plasma, it all depends of the first matter touched by the photons. This water in the pulp chamber has a temperature higher than 1500 degrees but only over a very short period of time: 30 microseconds. It’s photons absorption (excited at 2940 µm) in water, which generates a thermic state. But it is Erbium YAG laser which generates the less therm compared to other lasers. As a matter of fact, the longer the length of photons is high and the lower the photons are energetic.
Let's recap, we insert the tip into the water the water is sublimated in plasma at 1500 degrees, the plasma being in the water and boiling at 1500 degrees, the water turns into steam and creates a bubble: a bubble of vapor, this bubble grows big and consequently increases the liquid pressure of the pulp chamber. Some bubbles are amalgamated to each other to form larger ones, then they go down in the liquid and consequently in the main canal (Fig. 2).
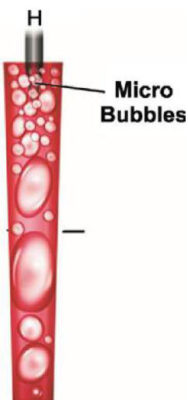
Laser activation and aqueous environment generates large bubbles that magnify and then explode. This expansion causes higher pressure in the fluids: it' s the cavitation effect[19].
The increase of the intraliquidian pressure is manifested by a visible phenomenon. The Venturi effect. The Venturi effect (from the name of the Italian physicist Giovanni Battista Venturi) is the given name to a phenomenon called fluid dynamics where gaseous or liquid particulars are accelerated due to a narrowing of their circulation area. The farther the tip is from the root canal entry, the more efficient this acceleration is.
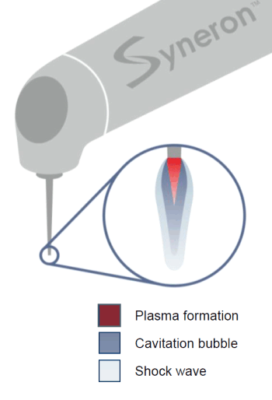
Just outside the end of the tip the irradiation energy of the Erbium YAG is almost absorbed in water to a depth of 10 µm. The water is immediately heated to a boiling temperature and transformed into steam in one microsecond. This bubble of water begins to expand and form a vacuum at the end of the tip. Since the vapor bubble expands to its expansion capacities, we believe that the continuous last emission passes through the vacuum and evaporates the surface of the water at the boundary of this bubble of water[20]-[21]. This is what we call the Moses effect[22]. But this vapour bubble cannot extend to infinity (forever) because the external pressure of the liquid exerts a contrary force to this expansion. When the bubble is at its maximum diameter, the external liquid pressure regain the top and collapses this bubble. When the irradiation stops, the bubble of vapor begins to shrink. The water surrounding the vapor bubble sinks strongly inside this bubble of vapor which decompresses. At the time of these violent collapse supersonic velocity waves (shock waves) are generated at the very beginning, then pressure waves at sound speed (acoustic waves) are generated secondly (Fig. 3)[23].
The shock waves are also called blast. Blast is a military term designating an explosion causing a suppression wave. This shock wave in the air strikes the person and causes a shock wave in his body(refraction): this internal shock wave can cause internal damage with delayed effects. More however a shock wave generated in water is more devastating than in the air, because water is incompressible.
During the collapse of the bubbles due to the interaction between the bubbles and their substrate and the interaction of the bubbles without their substrate, a jet of high speed liquid is formed[24]-[25]. These shockwaves and the movement (acoustic streaming) result in a high shear stress acting on the wall of the root canal. This eliminates debris and plays a key role in an increased cleaning efficiency[24bis]. After the first large vapor wave disappearance, abruptly the shock wave changes and largely modifies the water pressure around the tip of the laser, resulting in the nucleation of a number of new cavitation bubbles. This phenomenon is generally called the rebound effect[26]-[27].
Conclusion
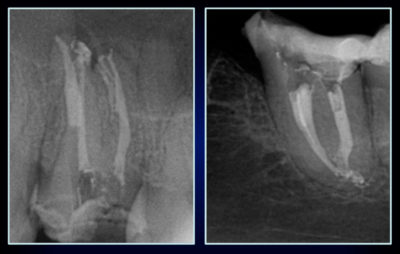
The very rapid formation of plasma creates the shockwave and the shockwave is more violent in the water than in the air because the air is incompressible. The shock waves increase the intracanal pressure and thus promotes a better removal of dentinal debris[24ter]. This physical observation is validated by various clinical in vitro studies, the one from Tokeda mentioned above and the latest studies of Drs Stabholtz and Sahar (Figs. 4 and 5)[28]. But if this cleaning is very efficient in the main and accessory canals what about the intratubular cleaning?
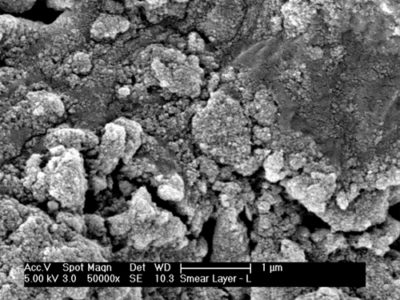
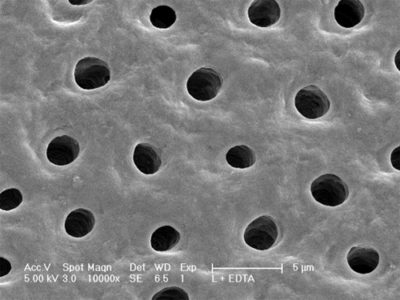
The cavitation effect : Gordon et al.[29] found that the cavitation effect allowed expansion and collapse of the intratubular water as deep as 1000 μm or more. But what about the effect of these shock waves on bacteria?
The aspiration of this intratubular water allows us to aspirate the bacteria presence in the dentinal tubules. The wavelength of 2940 nm is absorbed in the water of the bacterial cytoplasm, this generates an increase in the intra bacterial pressure, causing the bacterial lipid membrane to rupture. This micropulse induced by absorption has been able to produce strong enough acoustic waves to disrupt and destroy intratubular bacteria (Fig. 6).
These results are significant as bacteria have been identified at depths of 1000 µm (Kouchi and al.[30] and at depths of 800 µm for E. Faecalis (Fig. 7)).
Clinical application of the laser in endodontics




Hypochlorite action
We use sodium hypochlorite for its bactericidal action, the advantage derived from hypochlorite are multiple:
- The hypochlorite is disinfectant.
- The shock waves allow to diffuse it.
- The creation of a water plasma generates singled and tripled oxygen: these are very reactive molecules, this allows to hyper oxygenate the hypoclorite and to propel it.
- By heating hypochlorite, we make it more active. Some studies show that when we activate the erbium yag laser with sodium hypochlorite at 25 degrees in the pulp chamber, the hypochlorite temperature in the third apical can reach 40 degrees in 20 seconds activation[37].
Different studies converge to show that the Erbium YAG laser is superior to other conventional techniques or to activate irrigation solutions:
- The dissolution of the pulp tissue is much faster[31]-[32].
- There are more eliminated dentinal debris, thus a better cleaning[33].
- Better efficiency for the elimination of temporary intracanal medication such as calcium hydroxide[34].
- The laser has a powerful action on the hypochlorite activation[35].
- Better elimination of ductal and intratubular bacteria[36].
Conclusion
Long decried and controversial, the laser gradually takes its place in endodontics and especially the Erbium YAG which meets of the requirements and irrigation objectives of the endodontic disinfection, canal system, isthmus and dentinal tubules. The exacerbation of the irrigation dynamics will make it possible to transport the irrigant to the foramen, ensuring its disinfection,and by meeting the goals of modern endodontics this will upset our concepts of too often, “over preparation” and meet the criteria of tissue saving.
General practitioner in Villié-Morgon (France) since 1999.
Exclusive endodontist in Bron (France) since 2009.
University degree in anatomy and cranio-cervico-facial dissection of the Faculty of Medicine of Paris.
Exclusive endodontist.
Former university assistant in the hospital Paris 7.
Visiting professor in the Nova Southeastern University of Florida, United States.
Bibliography
1 Figdor D, Davies JK, Sundqvist G. Starvation survival, growth and recovery of Enterococcus faecalis in human serum. Oral Microbiol Immunol 2003;18: 234 –9
2 Sedgley CM, Lennan SL, Appelbe OK. Survival of Enterococcus faecalis in root canals ex vivo. Int Endod J 2005;38:735– 42.
3 Deutsch S. A preliminary study of the fluid mechanics of liquid penetrant testing. J Res Natl Bur Stand 1979;84:287–92.
4 Pesse AV, Warrier GR, Dhir VK. An experimental study of the gas entrapment process in closed-end microchannels. Int J Heat Mass Transf 2005;48:5150–65.
5 Luks S. Practical endodontics. Philadelphie : JB Lippincott, 1974 : 82-85.
6 Tay FR, Gu LS, Schoeffel GJ, Wimmer C, Susin L, Zhang K et al. Effect of vapor lock on root canal debridement by using a sidevented needle for positive-pressure irrigant delivery, J Endod 2010 ; 36 : 745-750.
7 Fazio R, Iacono S. Entrapped gas action for one-dimensional models of capillary dynamics. In: Proceedings of the World Congress on Engineering, July 1–3, 2009, London, vol. II. London: World Congress of Engineering; 2009.
8 Bankoff S, Baiche J. Entrapment of gas in the spreading of a liquid over a rough surface. AIChE J 1958;4:24–6
9/9bis Jorge Vera, DDS, Ana Arias and Monica Romero : Dynamic Movement of Intracanal Gas Bubbles during Cleaning and Shaping Procedures: The Effect of Maintaining Apical Patency on Their Presence in the Middle and Cervical Thirds of Human Root Canals—An In Vivo Study. JOE — Volume 38, Number 2, February 2012
10 Hess W. The Anatomy of the root-canals of the teeth of the permanent dentition. John Bale, Sons & Danielsson, Ltd., 1925 ;21-46
11 Peters OA, Schönenberger K, Laib A. Effects of four Ni-Ti preparation techniques on root canal geometry assessed by micro computed tomography. Int Endod J 2001 ; 34 : 221-230.
12 Hall-Stoodley L, Stoodley P. Biofilm formation and dispersal and the transmission of human pathogens, Trend Microbiol 2005 ; 13 : 7-1.
13/13bis Molven O, Olsen I, Kerekes K. Scanning electron microscopy of bacteria in apical part of root canals in permanent teeth with periapical lesions, Endod Dent Traumatol 1991 ; 7 : 226-229.
14 Costertoon W, Veeh R, Shirtliff M, Pasmore M, Post C, Ehrlich G. The application of biofilm science to the study and control of chronic bacterial infections. J Clin Invest 2003 ; 112 : 1466-1477.
15 Svensater G, Bergenholtz G. Biofilms in endodontic infections. Endod Topics.2004 ; 9 : 27-36.
16 Sedlacek MJ, Walker C. Antibiotic resistance in an in vitro subgingival biofilm model. Oral Microbiol Immunol 2007 ; 22 : 333-339.
17 Love RM, Jenkinson HF. Invasion of dentinal tubules by oral bacteria. Crit Rev Oral Biol Med 2002;13:171–83.
18 Takeda FH, Harashima T, Kimura Y, Matsumoto K. Comparative study about the removal of smear layer by three types of laser devices. J of Clinical Laser. 1998 ; 16 : 117-122.
19 Himeka Matsumoto, Yoshito Yoshimine, Akifumi Akamine, Visualization of Irrigant Flow and Cavitation Inducedby Er:YAG Laser within a Root Canal Model(J Endod 2011;37:839–843.
20 Ith M, Pratisto H, Altermatt HJ, Frenz M, Weber HP. Dynamics of laser-induced channel formation in water and influence of pulse duration on the ablation of biotissue under water with pulsed erbium-laser radiation. Appl Phys B 1994;59:621–9.
21 Shori RK, Walston AA, Stafsudd OM, Fried D, Joseph T, Walsh JT Jr. Quantification and modeling of the dynamic changes in the absorption coefficient of water at l = 2.94 mm. IEEE 2001;7:959–70.
22 van Leeuwen TG, van de Veen MJ, Verdaasdonk RM, Borst C. Noncontact tissue ablation by holmium:YSGG laser pulses in blood. Lasers Surg Med 1991;11:26–34.
23 Flotte TJ, Doukas A. Laser induced pressure effects. SPIE, Laser Tissue Interaction 1992;1646:295–300.
24/24bis/24ter Song WD, Hong MH, Lukyanchuk B, Chong TC. Laser-induced cavitation bubbles for cleaning of solid surfaces. J Appl Phys 2004;95:2952–6.
25 Brujan EA. Cardiovascular cavitation. Med Eng Phys 2009;31:742–51.
26 Himeka Matsumoto, Yoshito Yoshimine, Akifumi Akamine, Visualization of Irrigant Flow and Cavitation Inducedby Er:YAG Laser within a Root Canal Model. J Endod 2011;37:839–843
27 Blanken J,DeMoor RJ, MeireM,Verdaasdonk R (2009) Laser induced explosive vapor and cavitation resulting in effective irrigation of the root canal. Part 1: a visualization study. Lasers Surg Med.
28 Sharonit Sahar-Helft, Aysxe Sena Kabasx Sarp, Adam Stabholtz, Vitaly Gutkin, Idan Redenski, Doron Steinberg. Comparison of Positive-Pressure, Passive Ultrasonic, and Laser-Activated Irrigations on Smear-Layer Removal from the Root Canal Surface. Photomedicine and Laser Surgery Volume 33, Number 3, 2015.
29 Gordon W, Atabakhsh VA, Meza F, Doms A, Nissan R, Rizoiu I, Stevens R: The antimicrobial efficacy of the erbium,chromium:yttrium-scandium-gallium-garnet laser with radial emitting tips on root canal dentin walls infected with Enterococcus faecalis. JADA 138:7:992–1002 (2007).
30 Kouchi Y, Ninomiya J, Yasuda H, Fukui K, Moriyama T, Okamoto H: Location of streptococcus mutans in the dentinal tubules of open infected root canals. J Dent Res 59:2038–2046 (1980).
31 Er:YAG Laser Activation of Sodium Hypochlorite for Root Canal Soft Tissue Dissolution, Katharina Kuhn, Heike Rudolph, Ralph G. Luthardt, Karl Stock, Rolf Diebolder and Raimund Hibst.
32 Mehmet Burak Guneser, Dilara Arslan, Aslihan Usumez. Tissue Dissolution Ability of Sodium Hypochlorite Activated by Photon-initiated Photoacoustic Streaming Technique. J Endod 2015;1–4
33 de Groot SD, Verhaagen B, Versluis M, Wu MK, Wesselink PR, van der Sluis LW (2009) Laser-activated irrigation within root canals: cleaning efficacy and flow visualization. Int Endod J
34 H. Arslan, M. Akcay, I. D. Capar, G. Saygili, T. Gok & H. Ertas.An in vitro comparison of irrigation using photon-initiated photoacoustic streaming, ultrasonic, sonic and needle techniques in removing calcium hydroxide. International Endodontic Journal, Volume 48, Issue 3, pages 246–251, March 2015
35 Macedo RG,Wesselink PR, Zaccheo F, Fanali D, van der Sluis LW. (2010) Reaction rate of NaOCl in contact with bovine dentine: effect of activation, exposure time, concentration and pH. International Endodontic Journal 43, 1108–15.
36 Evaluation of the Bactericidal Effect of Nd:YAG, Er:YAG, Er,Cr:YSGG Laser Radiation, and Antimicrobial Photodynamic Therapy (aPDT) in Experimentally Infected Root Canals. Xiaogang Cheng et al. Lasers in Surgery and Medicine 44:824–831 (2012).
37 Etudes publiées en 2011 par le Pr Tomov. G à la Faculté de Médecine Dentaire de Sofia, Bulgarie.
38 Endal, Shen, Knut, Gao & Haapasalo. A high-resolution Computed Tomographic Study of changes in root canal isthmus area by instrumentation and root filling. J Endod 2011 ; 37 : 223-227.