Dr. David Guex
November 2015 - Dentoscope n°153
Download the PDF
Today, we note the multiplication of scientific articles describing the activation of the irrigation solutions by the use of an Erbium YAG laser. Currently users of this technology find fewer postoperative pains and they practice less surgery. Indeed, after classical instrumentation and irrigation they note the absence of ductal debris raised by the conventional techniques. Then if they use Erbium YAG laser to activate the irrigants, then new debris appear in the solutions. How can we explain this phenomenon?
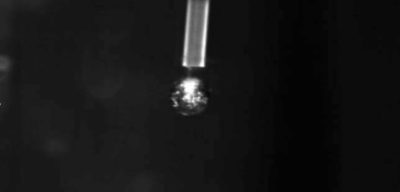
The disinfectant solution used in endodontics is sodium hypochlorite. It has a concentration between 2,5% and 6%. But it's above all a dilution in water. When we put the laser tip into the solution contained in the pulp cavity and we press down on the pedal of the machine, the chamber generates a series of excited photons at a precise wavelength: 2940 nm. The molecules intrinsically have absorption curves and it happens that this wavelength of 2940 nm is maximally absorbed (peak absorption) by water. When the excited photons of 2940 nm meet a water molecule this one will be sublimated. Erbium YAG laser induces the implosion of the water molecules. This sublimation of matter is called Plasma; (Fig.1).
Different studies converge to show the efficiency of the Erbium YAG laser to activate irrigation solutions. The elimination of ductal and intratubular bacteria is thus increased.
The plasma corresponds to the fourth element constituting the universe, the other three being the liquid elements, gaseous and solid. Our sun is a Plasma. In fact the plasma is not emitted by the end of the tips, it's a transformation of matter by photonic energy. There are several different plasmas: water, dentin, blood, depending on the nature of the material that has been exposed to the photons. This water plasma in the pulp chamber at a temperature higher than 1500 degrees, but over a very short duration of a few microseconds. It's the absorption of excited photons at 2940 nm in the water which generates thermical state. However the Erbium YAG laser generates less therm than the others.
Indeed, the more the wavelength is high and the less the photons are energetic. Let's recap: we inserts the tips into the water, the water is sublimated into plasma at 1500 degrees, this one being in water at 1500 degrees, the water turns into steam and creates a bubble. This bubble of vapor gets fatter and increases the liquid pressure of the pulp chamber, then in the root canal system. These bubbles are amalgamated with each other increasing in volume, then explode, by generating a high pressure in the fluids[1], this is called, cavitation; (Fig.2)
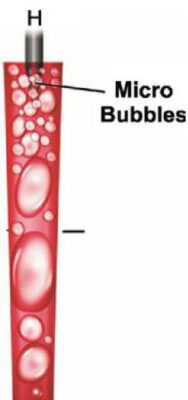
Just outside the end of the tip the irradiation energy if the Erbium YAG is almost absorbed in water to a depth of 5µm or so, the water is immediately heated to a boiling temperature and transformed into steam in a microsecond. This bubble of vapour begins to expand and form an empty space in front of the end of the tip. As the bubble of vapor expands to its expansion possibilities, we believe that the continuous emission goes through the empty space and evaporate the surface of the water at the boundary of this bubble of water[2]-[3]. This is what we call the Moses effect[4]. But this bubble of vapour cannot extend to infinity because the external pressure of the liquid exerts a contrary force to this expansion. When the bubble is at its maximum volume to external liquid pressure regain the top and collapse this bubble.
A shock wave generated in water is more devastating than in the air because water is incompressible.
When the irradiation stops the bubble of water begins to shrink, the water surrounding the bubble of vapor sinks strongly inside of the bubble which decompresses. At the very moment of this violent collapse, pressure waves are generated, in the beginning supersonic speeding waves (shock waves) and secondly pressure waves at the speed of sound (acoustic waves)[5]; (Fig.3).These shock waves are also called "Blast". Blast is a military term designating an explosion causing a suppression wave. This shock wave in the air strikes the person causing a shock wave in his body (refraction), this shock wave can cause internal damages with delayed effects. More over a shock wave generated in water is more devastating than in the air because water is incompressible. During the collapse of the bubbles due to the interaction of the bubbles without their substrate, a jet of a high speed liquid is formed[6]-[7].These shock waves and the fast liquid movement,(acoustic streaming) results in a high shear stress acting on the wall of the root canal, this eliminates debris and plays a key role in an increased cleaning[6bis]. After the big disappearance of the vapor bubbles, the shock wave changes suddenly and largely modifies the water pressure around the tip of the laser, resulting in the nucleation of a number of new cavitation bubbles[8], the phenomenon is generally called the rebound effect[9].
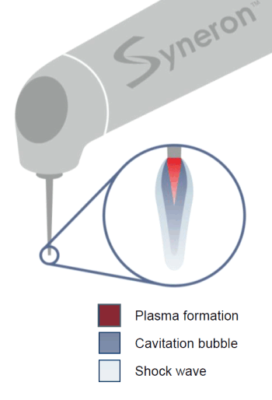
To sum up: The very rapid formation of plasma creates the shock wave which is more violent in the water than in the air because water is incompressible. The shock wave increases the intracanal pressure and thus helps a better removal of the dentinal debris[6]. The increase of the inter-fluid pressure is manifested by a visible phenomenon: The Venturi effect. The Venturi effect (from the name of the Italian physicist Giovanni Battista Venturi) is a phenomenon of the dynamics of the fluids where gaseous or liquid particles are accelerated because of a narrowing of their circulation areas. The more the tips is far from the canal entrance and the more efficient this acceleration is.
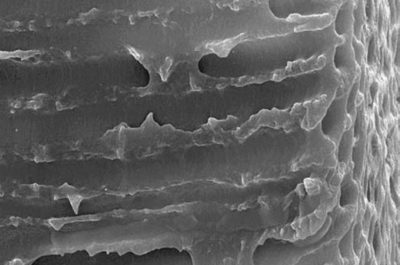
The elimination of intra canal debris is validated by different clinical studies in vitro. In 1998, Hirono Takeda[10] showed that in endodontics, the most effective laser is the Erbium-YAG laser for the removal of debris and mud (Smear layer).This observation is validated by the latest studies of Drs Stabholtz and Sahar; (Figs 4 and 5[11]).
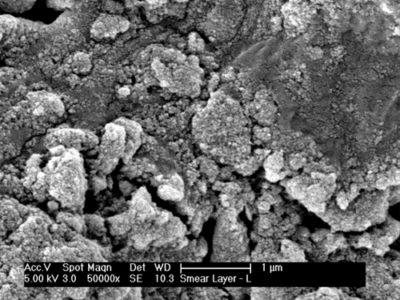
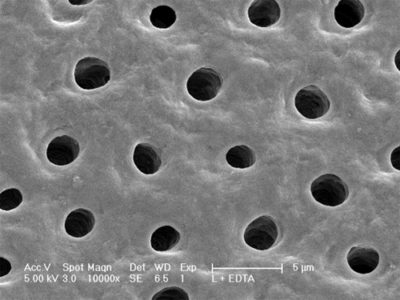
But if this cleaning is very effective in the main and accessory channels, what about the intra-tubular cleaning? Gordon et al.[12] found that the cavitation effect allowed the expansion and collapse of the intra-tubular water to a depth of 1000 μm, maybe much more. This collapse of intra-tubular water is probably the most important phenomenon of all those described above and in the cleaning of the endodond. (Fig. 6)
But what about the effect of these shock waves on bacteria?
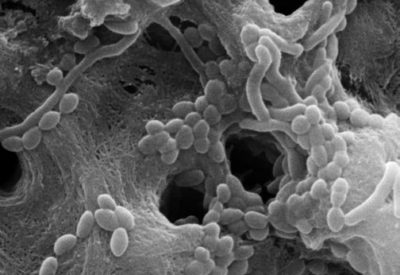
This micro pulse, made by absorption, has been able to produce strong enough acoustic waves to disrupt and destroy intra-tubular bacteria (Fig. 7). These results are significant since the bacteria have been identified at depths of 1000 μm[13] and at depths of 800 μm for E. Faecalis. But we can ask a legitimate question, does the power generated by the Erbium-YAG laser can propel liquids outside the peri-apex? The answer is no. Why? Initially, we don't have to mix in vitro studies on extracted teeth and clinical findings under in vitro operating microscope. In 10 years of use of the Erbium YAG laser, I have never seen a liquid filling the pulp chamber that is siphoned beyond the peri-apex, by its use. The first explanation is anatomical: because the roots are surrounded by a periondontal ligament and bone. The endodond behaves as a closed-end canal or as a tube producing a gas-locking effect contained in the liquid[14]-[15]. On the other hand the periodontal ligament is vascularized, there is an arterial pressure in this ligament which opposes the intracanal fluid pressure. The peri-apex pressure counterbalances that of the laser. If the liquid pressure generated by the laser is greater than the ligament, or if the ligament is weakened because inflammatory, the first clinical result observed is an instantaneous bleeding. In reaction we decrease the energy transmitted in the liquid.
Action on hypochlorite
We use sodium hypochlorite for its bactericidal action. Its advantages are multiple:
- Hypochlorite is disinfectant
- Shock waves make it possible to spread it
- The creation of a water plasma generates singulated and tripled oxygen: these are very reactive molecules, this allows to hyper-oxygenate the hypochlorite and to propel it.
- By heating the hypochlorite we make it more active. Professor Tomov's studies show that when we activate sodium hypochlorite at 25 degrees in the pulp chamber with this laser, the temperature of the hypochlorite in the apical third rose to 40 degrees after 20 seconds of activation.
Different studies converge to show that this laser is superior to other conventional techniques to activate irrigation solutions. The dissolution of pulp tissues is much faster[16]-[17].There is more eliminated dentinal debris, the endodond is cleaner[18]. The same goes for the elimination of temporary intra-ductal medications such as calcium hydroxide[19]. The laser has a powerful action on The activation of hypochlorite[20]. The elimination of ductal and intra-tubular bacteria is increased[21].
General practitioner in Villié-Morgon (France) since 1999.
Exclusive endodontist in Bron (France) since 2009.
University degree in anatomy and cranio-cervico-facial dissection of the Faculty of Medicine of Paris.
Bibliography
1 Himeka Matsumoto, Yoshito Yoshimine, Akifumi Akamine, Visualization of Irrigant Flow and Cavitation Inducedby Er:YAG Laser within a Root Canal Model, J Endod 2011;37:839–843.
2 Ith M, Pratisto H, Altermatt HJ, Frenz M, Weber HP. Dynamics of laser-induced channel formation in water and influence of pulse duration on the ablation of biotissue under water with pulsed erbium-laser radiation. Appl Phys B 1994;59:621–9.
3 Shori RK, Walston AA, Stafsudd OM, Fried D, Joseph T, Walsh JT Jr. Quantification and modeling of the dynamic changes in the absorption coefficient of water at l = 2.94 mm. IEEE 2001;7:959–70.
4 Van Leeuwen TG, van de Veen MJ, Verdaasdonk RM, Borst C. Noncontact tissue ablation by holmium:YSGG laser pulses in blood. Lasers Surg Med 1991;11:26–34.
5 Flotte TJ, Doukas A. Laser induced pressure effects. SPIE, Laser Tissue Interaction 1992;1646:295–300.
6/6bis Song WD, Hong MH, Lukyanchuk B, Chong TC. Laser-induced cavitation bubbles for cleaning of solid surfaces. J Appl Phys 2004;95:2952–6.
7 Brujan EA. Cardiovascular cavitation. Med Eng Phys 2009;31:742–51.
8 Blanken J, DeMoor RJ, MeireM, Verdaasdonk R (2009) Laser induced explosive vapor and cavitation resulting in effective irrigation of the root canal. Part 1: A visualization study. Lasers Surg Med.
9 Himeka Matsumoto, Yoshito Yoshimine, Akifumi Akamine, Visualization of Irrigant Flow and Cavitation Inducedby Er:YAG Laser within a Root Canal Model. J Endod 2011;37:839–843.
10 Takeda FH, Harashima T, Kimura Y, Matsumoto K. Comparative study about the removal of smear layer by three types of laser devices. J of Clinical Laser. 1998 ; 16 : 117-122.
11 Sharonit Sahar-Helft, Aysxe Sena Kabasx Sarp, Adam Stabholtz, Vitaly Gutkin, Idan Redenski, Doron Steinberg. Comparison of Positive-Pressure, Passive Ultrasonic, and Laser-Activated Irrigations on Smear-Layer Removal from the Root Canal Surface. Photomedicine and Laser Surgery Volume 33, Number 3, 2015.
12 Gordon W, Atabakhsh VA, Meza F, Doms A, Nissan R, Rizoiu I, Stevens R: The antimicrobial efficacy of the erbium, chromium: yttrium-scandium-gallium-garnet laser with radial emitting tips on root canal dentin walls infected with Enterococcus faecalis. JADA 138:7:992–1002 (2007).
13 Kouchi Y, Ninomiya J, Yasuda H, Fukui K, Moriyama T, Okamoto H: Location of streptococcus mutans in the dentinal tubules of open infected root canals. J Dent Res 59:2038–2046 (1980).
14 Tay FR, Gu LS, Schoeffel GJ, et al. Effect of vapor lock on root canal debridement by using a side-vented needle for positive-pressure irrigant delivery. J Endod 2010;36: 745–50.
15 Senia ES, Marshall JF, Rosen S. The solvent action of sodium hypochlorite on pulptissue of extracted teeth. Oral Surg Oral Med Oral Pathol 1971;31:96–103.
16 Er:YAG Laser Activation of Sodium Hypochlorite for Root Canal Soft Tissue Dissolution, Katharina Kuhn, Heike Rudolph, Ralph G. Luthardt, Karl Stock, Rolf Diebolder and Raimund Hibst.
17 Mehmet Burak Guneser, Dilara Arslan, Aslihan Usumez. Tissue Dissolution Ability of Sodium Hypochlorite Activated by Photon-initiated Photoacoustic Streaming Technique. J Endod 2015;1–4.
18 De Groot SD, Verhaagen B, Versluis M, Wu MK, Wesselink PR, van der Sluis LW (2009) Laser-activated irrigation within root canals: cleaning efficacy and flow visualization. Int Endod J.
19 H. Arslan, M. Akcay, I. D. Capar, G. Saygili, T. Gok & H. Ertas.An in vitro comparison of irrigation using photon-initiated photoacoustic streaming, ultrasonic, sonic and needle techniques in removing calcium hydroxide. International Endodontic Journal, Volume 48, Issue 3, pages 246–251, March 2015.
20 Macedo RG,Wesselink PR, Zaccheo F, Fanali D, van der Sluis LW. (2010) Reaction rate of NaOCl in contact with bovine dentine: effect of activation, exposure time, concentration and pH. International Endodontic Journal 43, 1108–15.
21 Evaluation of the Bactericidal Effect of Nd:YAG, Er:YAG, Er,Cr:YSGG Laser Radiation, and Antimicrobial Photodynamic Therapy (aPDT) in Experimentally Infected Root Canals. Xiaogang Cheng et al. Lasers in Surgery and Medicine 44:824–831 (2012).